In recent years, herpes viruses (from the Greek herpes - creeping) have become increasingly important in infectious pathology. The attention that virologists and clinicians have shown over the past 25 years to human herpesvirus diseases is associated with their significant epidemiological role and social significance in the modern world. The steady increase in the number of herpes diseases in adults and children necessitates a comprehensive study of herpes infection and the development of effective methods for the prevention and treatment of various forms of this infection. Among viral infections, herpes occupies one of the leading places due to the ubiquity of viruses, the variety of clinical manifestations, as a rule, a chronic course, as well as various ways of transmitting viruses.
It is among the most common and poorly controlled human infections. Herpes viruses can circulate in a body with a normal immune system asymptomatically, but in immunosuppressed people they cause severe illness and death. According to WHO, mortality from herpes infection among viral diseases is in second place (15.8%) after hepatitis (35.8%).
Herpes viruses are united in an extensive family herpesviridae and are currently the most clearly classified. Family herpesviridae includes more than 80 representatives, 8 of which are the most pathogenic for humans (human herpes virus-HHV). Herpes viruses, a phylogenetically ancient family of large DNA viruses, are divided into 3 subfamilies depending on the type of cells in which the infectious process occurs, the nature of virus reproduction, genome structure, molecular biological and immunological features: α, β and γ ( , according to N. G. Perminov, I. V. Timofeev et al., State Scientific Center for Virology and Biotechnology).
α-herpesviruses, including HSV-1, HSV-2 and VZV, are characterized by rapid viral replication and cytopathic effect on cultures of infected cells. Reproduction of α-herpesviruses occurs in various cell types, viruses can remain in a latent form, mainly in the ganglia.
β-herpes viruses are species-specific, affecting different kinds cells that increase in size (cytomegaly) can cause immunosuppressive conditions. Infection can take a generalized or latent form; persistent infection easily occurs in cell culture. This group includes CMV, HHV-6, HHV-7.
γ-herpes viruses are characterized by tropism for lymphoid cells (T- and B-lymphocytes), in which they persist for a long time and which can transform, causing lymphomas, sarcomas. This group includes Epstein-Barr virus and HHV-8-herpes virus associated with Kaposi's sarcoma (KSHV). KSHV is the closest in genomic organization to the T-cell-tropic simian herpes virus (HVS).
Herpes viruses are associated with malignancy and are able (at least EBV and HVS) to transform cells in vitro. All herpes viruses are similar in morphological features, size, type nucleic acid(double-stranded DNA), icosadeltahedral capsid, the assembly of which occurs in the nucleus of an infected cell, the membrane, the type of reproduction, the ability to cause chronic and latent infection in humans.
Cloning of herpes viruses occurs according to the following scheme: spontaneous random adsorption of the original "mother" virus on the surface of the target cell, "undressing of the virion" - splitting of the envelope and capsid, infiltration viral DNA into the nucleus of the target cell, the formation and maturation of "daughter" virions by budding on the nuclear membrane. After a cell is infected, for example, with herpes simplex virus types 1 or 2, the synthesis of new viral proteins begins after 2 hours, and their number reaches a maximum after about 8 hours. amino acids, proteins, lipoproteins and nucleosides. These molecules enter the infected cell from the interstitial spaces as the intracellular reserves are depleted. In this regard, viruses depend on the intensity of intracellular metabolism, which, in turn, is determined by the nature of the target cell. The highest metabolic rate is characteristic of short-lived cells of the epithelioid type; therefore, herpes viruses colonize cells of the epithelium and mucous membranes, blood and lymphatic tissues especially well. Completely formed and ready for subsequent active reproduction, “daughter” infectious virions appear inside the infected cell after 10 hours, and their number becomes maximum after about 15 hours. The number of virions to a certain extent affects the rate of infection spread and the area of damage.
The first generation of "daughter" herpes viruses begins to enter the environment (intercellular spaces, blood, lymph and other biological media) after about 18 hours. This can be observed in clinical practice with uncontrolled processes (for example, with chickenpox, herpes zoster, generalization cytomegalovirus infection) - elements of a herpetic rash appear on the skin or mucous membranes in waves. Herpes viruses are in a free state for a very short period (from 1 to 4 hours) - this is the duration that is typical for the period of acute intoxication in herpes virus infections. The life span of each generation of formed and adsorbed herpes viruses averages 3 days.
In epidemiological terms, the following information about herpes viruses is most interesting: virions are extremely thermolabile - they are inactivated at a temperature of 50-52 ° C for 30 minutes, at a temperature of 37.5 ° C - for 20 hours, stable at a temperature of 70 ° C; well tolerate lyophilization, long-term stored in tissues in a 50% solution of glycerin. On metal surfaces (coins, door handles, water faucets), herpes viruses survive for 2 hours, on plastic and wood - up to 3 hours, in wet medical cotton wool and gauze - until they dry at room temperature (up to 6 hours).
The unique biological properties of all human herpes viruses are tissue tropism, the ability to persistence and latency in the body of an infected person. Persistence is the ability of herpes viruses to continuously or cyclically multiply (replicate) in infected cells of tropic tissues, which creates a constant threat of the development of an infectious process. The latency of herpes viruses is the lifelong persistence of viruses in a morphologically and immunochemically modified form in the nerve cells of the regional (in relation to the place of introduction of the herpes virus) ganglia of sensory nerves. The strains of herpes viruses have different ability to persistence and latency and sensitivity to antiherpetic drugs due to the peculiarities of their enzyme systems. Each herpes virus has its own rate of persistence and latency. Among those studied, the most active in this respect are herpes simplex viruses, the least active is the Epstein-Barr virus.
According to numerous studies, by the age of 18, more than 90% of urban residents are infected with one or more strains of at least 7 clinically significant herpes viruses (herpes simplex types 1 and 2, varicella zoster, cytomegalovirus, Epstein-Barr, human herpes types 6 and 8 ). In most cases, primary and re-infection occurs by airborne droplets, by direct contact or through household and hygiene items (shared towels, handkerchiefs, etc.). Oral, genital, orogenital, transfusion, transplantation and transplacental routes of infection transmission have also been proven.
Herpes virus infections are widespread in the world and tend to grow steadily. A feature of herpes virus infection is the possibility of involving many organs and systems in the infectious process, which is the reason for the variety of diseases caused by herpes viruses, ranging from simple mucocutaneous to life-threatening generalized infections. An important property of herpes viruses is the ability, after primary infection in childhood, to persist for life in the body and reactivate under the influence of various exogenous and endogenous provoking factors.
Human infection with these herpes viruses is accompanied by clinical symptoms of the corresponding acute infectious disease in an average of no more than 50% of people, mainly in children: sudden erythema (human herpes virus type 6), aphthous stomatitis (herpes simplex viruses types 1 or 2), chickenpox (varicella zoster virus), infectious mononucleosis (Epstein-Barr virus), mononucleosis-like syndrome (cytomegalovirus). In the remaining patients, the infection is asymptomatic, which is especially true for adolescents and adults. In addition to the biological properties of the herpes virus strain, the course of acute and recurrent herpes viral diseases is influenced by individual (age, sex, phylo- and oncogenetic) features of the immune response of an infected person to numerous virus antigens.
Often, especially with a decrease in the body's immunoreactivity, herpes viruses act as opportunistic viruses, leading to a more severe course of the underlying disease with unusual clinical manifestations. Herpes simplex viruses types 1 and 2, as well as CMV, are among the causative agents of TORCH infections. They play an important role in the violation of human reproductive function, the development of serious diseases of the mother, fetus, newborn and young children.
Diseases caused by HSV, CMV, EBV viruses are considered as AIDS indicator due to their frequent detection in this pathology. In 1988 they were included in the expanded definition of cases subject to epidemiological surveillance for AIDS. The results of recent studies indicate the role of some herpes viruses (HHV-8, CMV, EBV, etc.) in the development of a number of malignant neoplasms: nasopharyngeal carcinoma, Burkitt's lymphoma, B-cell lymphoma, breast cancer, adenocarcinoma of the intestine and prostate, cervical carcinoma cervical canal, Kaposi's sarcoma, neuroblastoma, etc.
Herpetic neuroinfections pose the greatest threat to health (mortality reaches 20%, and the incidence of disability is 50%), ophthalmoherpes (in almost half of patients it leads to the development of cataracts or glaucoma) and genital herpes.
Apparently, all known herpes virus infections can recur, but the threshold and reasons for the transformation of an acute form into a recurrent one for each type of herpes virus are different. In general, herpes virus infections take a recurrent course in no more than 8-20% of patients. Recurrent herpes virus diseases in some people can be perceived as "chronic" when they develop over many years, not only destroying physical health and the functions of vital systems, but also psychologically extremely adversely affecting the patient. Therefore, for practical purposes, herpes virus infections are classified taking into account both the localization of the process, recurrence and etiology ( ).
The causes of the recurrent course of herpes virus infections are diverse. One of them is that the transformation of an acute herpes virus process into a chronic one occurs with the explicit “connivance” of the immune system. If acquired immunodeficiency as a result of chemotherapy or HIV infection is easily explained, then all attempts to find out what causes the main defect in the immune response in immunologically healthy people with a recurrent course of herpes virus infection have been unsuccessful. Another reason is, apparently, in the quantitative and qualitative features of the persistence and latency of a particular strain of the herpes virus in the patient's body.
All virus detection and identification methods are based on the following principles:
Electron microscopy: rapid diagnosis allows you to detect HS or their components directly in samples taken from the patient, and give a quick answer in a few hours. The causative agent is detected using electron microscopy of clinical material with negative contrast.
Serological methods are inferior in terms of information content and sensitivity to other methods of laboratory diagnostics and do not allow establishing the etiology of a particular form of the disease with a sufficient degree of certainty. An increase in antibody titers occurs
late (several weeks) after infection or reactivation of the virus, and at the same time, it may not be observed in immunodeficient individuals. To establish a 4-fold increase in the titer of antibodies to herpes virus infection (an indicator of primary infection), it is necessary to study paired sera. Serological reactions (RSK, RN) have a high specificity, but relatively low sensitivity, and, moreover, are difficult to set up.
The immunofluorescent method, ELISA, RAL, and IB have received wide practical application.
The most accurate method for diagnosing herpes virus infection is the isolation of the virus from various cell cultures.
To detect the herpes virus, molecular biological methods are used: polymerase chain reaction and molecular hybridization reaction, which make it possible to detect the presence of viral nucleic acid in the test material. PCR can be considered the most sensitive and fastest reaction. The sensitivity of the method makes it possible to determine one molecule of the desired DNA in samples containing 10 cells.
The treatment of herpes infection remains a challenge to date. The chronic course of the process leads to the immune restructuring of the body: the development of secondary immune deficiency, inhibition of the reaction of cellular immunity, and a decrease in the body's nonspecific defenses. Despite the variety of drugs used to treat herpes infection, there are no drugs that provide a complete cure for herpes. Herpes virus infection is one of the most difficult to control diseases. This is due, first of all, to the variety of clinical lesions, the development of drug resistance of the virus, and the presence of molecular mimicry in herpes viruses. Therefore, for the successful treatment of herpes infection, it is necessary to choose the right antiviral drug, its dose and duration of treatment, and use a combination of various drugs. In order to increase the effectiveness of treatment, it is also necessary to include immunobiological preparations that help correct the immune status, as well as pathogenetic agents that alleviate the patient's condition, in the treatment regimens to improve the effectiveness of treatment.
Currently, all antiherpetic drugs are divided into 3 main groups of antiviral drugs ( ).
The mechanism of action of chemotherapy drugs (abnormal nucleosides: Valtrex, Vectavir, Famvir, Cymevene) is associated with inhibition of viral DNA synthesis and viral replication by competitive inhibition of viral DNA polymerase.
In immunomodulating drugs (alpizarin, imunofan, licopid, polyoxidonium), active substances have immunostimulatory properties in relation to cellular and humoral immunities, redox processes, and cytokine synthesis.
IFN inducers (amiksin, neovir, cycloferon) combine etiotropic and immunomodulatory effects. The drugs induce the formation of endogenous IFN (α, β, γ) by T- and B-lymphocytes, enterocytes, hepatocytes.
A special place among the means of anti-herpes virus therapy is occupied by a herpes vaccine for the activation of cellular immunity, its immunocorrection in the remission phase. Vaccination has 2 goals: prevention of primary infection and the occurrence of a state of latency, as well as prevention or alleviation of the course of the disease.
However, despite the existence of an extensive list of antiherpetic drugs, herpes is still a poorly controlled infection. This is due to the genotypic characteristics of the pathogen, and the long-term persistence of the virus in the body, and the formation of strains resistant to antiviral drugs. The maximum clinical effect can be obtained only with rational complex therapy of drugs with different mechanisms of action.
The St. Petersburg group of virologists and infectious disease specialists headed by V. A. Isakov proposed a program for the treatment and prevention of herpes infection (Table 4).
Advantages of complex therapy of GI.
Thus, GI therapy is a complex and multicomponent task.
For literature inquiries, please contact the editor.
T. K. Kuskova, Candidate of Medical Sciences
E. G. Belova, Candidate of Medical Sciences
MGMSU, Moscow
General properties:
"once infected - infected for life".
In certain cells, they are stored as copies of circular DNA autonomously from chromosomes (non-integrative virogeny). Allocate: latent infection and reactivation.
Morphology:
Virion size - from 100 to 300 nm;
Nucleocapsid (core) of cubic symmetry, supercapsid, amorphous layer (tegument);
Nucleocapsid - 162 capsomeres;
Linear double-stranded viral DNA;
70-200 functional and structural proteins:
super early,
Late.
About 30 glycoproteins:
Superficial and capsid;
- DNA polymerase.
antigenic properties. Glycoproteins of the outer shell are type-specific antigens, nucleocapsid proteins are group-specific antigens.
Treatment of herpesvirus infections: a cyclovir, ganciclovir - suppression of DNA polymerase, ribavirin - suppression of enzymes that provide capping of viral mRNA.
Herpes simplex virus (HSV):
HSV-1 (labial herpes) and
HSV-2 (genital herpes).
Cultivation:
tissue culture, CPD;
chicken embryos - infection in the chorion-allantoic membrane → plaques (HSV-1 - small plaques, HSV-2 - large);
organism of laboratory animals: mice, rats, guinea pigs, hamsters, rabbits, dogs, monkeys. More often - infection of rabbits (intranasally or in the cornea of the eye) or suckling mice (in the brain).
HSV1 pathogenesis.
Source of infection- a sick person in a latent or active form.
Mechanism of infection- contact.
entrance gate- oral mucosa, nose and damaged skin.
Primary contamination- in early childhood upon contact with infected saliva (aphthous, vesicular-erosive gingivostomatitis).
The virus enters through the nerve endings regional ganglia of sensory nerves(trigeminal ganglia), where it is stored in the nuclei of neurons in the form of circular DNA, periodically emigrates to the periphery asymptomatically or with reactivation.
The virus may take an ascending path → encephalitis.
Reactivation: Sunburn, infections, immunosuppression, emotional stress, menstruation, trigeminal nerve surgery, immunosuppressive drugs, organ transplants.
Clinical manifestations of HSV-1 reactivation: labial herpes, skin herpes (especially of the face), keratoconjunctivitis (ophthalmic herpes).
HSV2 pathogenesis:
HSV-2- tropism for the epithelium of the genital area.
Primary infection - sexually.
Asymptomatic infection → regional ( sacred) ganglia of the posterior roots of the spinal cord.
Only 1-15% of those infected after 2-3 days develop vesicular-erosive rashes on the erytomatous-edematous mucous membrane of the genital organs.
Special danger for fetus(TORC H). The fetus becomes infected in the birth canal → generalized herpes. C-section.
sanogenesis
When infected - antiviral antibodies, but the virus in the presence of specific antibodies does not lose its infectivity.
The main role in antiviral protection in herpes infection is CTL.
Tendency to generalization of herpes in patients with defects in T-cell immunity.
Microbiological diagnostics:
It is carried out with erased or hidden forms, in the prenatal period
Material: discharge from rashes, blood.
cytological method (Zank test) - identification of characteristic multinucleated giant cells with inclusion bodies. REEF.
Virological method: isolation of the virus in various cell cultures, followed by its identification in the reactions of ELISA, RN, RIF. PCR.
Serological method: AT in ELISA. AT classes, avidity index. AT to the "early" proteins of viruses.
Treatment and prevention:
For severe lesions, prescribe acyclovir.
Vaccine herpetic culture inactivated contains HSV1 and HSV2, is used to treat patients with herpetic lesions in remission not earlier than 2 weeks after the disappearance of the clinical manifestations of herpes, with ophthalmoherpes not earlier than 1 month.
Vaccination reduces the frequency of recurrence of herpes infection.
Varicella-Zoster Virus:
HHV3: Varicella zoster and herpes zoster virus -Varicella-ZosterVirus, (VOG,VZV).
The varicella-zoster virus causes a common childhood infection - chicken pox or chickenpox, persisting in sensitive ganglia, the virus is reactivated in the form of herpes zoster (herpes zoster), manifested by neuralgia and rashes along the nerve trunks.
PathogenesisVZV infections
Usually get sick children(usually 5-9 years), often easy, without complications. Adults are harder, with complications.
Source of infection- a sick man. The patient is contagious 24 hours before the onset of the rash and throughout the entire period of the rash.
Mechanism aspiration infection, path infection - airborne.
entrance gate- epithelium of the upper respiratory tract → primary replication → blood → generalization.
Main target - cells basal layer of the epidermis. The main symptom is exanthema on the skin of the trunk, less often on the face, neck, limbs, enanthema.
The most likely complication is a secondary pyogenic infection of the vesicles. 15% of adults have pneumonia. Post-infectious encephalitis and meningitis may develop.
PathogenesisVZV infections
Maybe transplacental infection of the fetus from a woman who got chickenpox during pregnancy.
If less than 5 days pass from the moment of infection to delivery, the born child may get sick severe form of chickenpox.
Chickenpox in the early months of pregnancy can cause severe fetal anomalies, and at a later date premature birth.
After recovery, the virus enters regional ganglia(any level of the spinal cord, trigeminal and facial nerves) and persists in
neurons in the form of circular DNA.
When exposed to an irritant
factor - reactivation - herpes zoster.
sanogenesis
After suffering from chickenpox, immunity for life.
Providing resistance to recurrence of chicken pox (ie, to a generalized process), AT does not save from local manifestations of virus reactivation.
Hypersensitivity to OG in the elderly and patients with defects in cellular immunity.
Material: the contents of skin rashes, discharge of the mucous membrane of the nasopharynx and blood serum.
cytological method: in smears-imprints from foci of skin lesions, stained according to Romanovsky-Giemsa or hematoxylin and eosin, multinuclear giant cells with intranuclear inclusions.
Virological method: isolation of the virus in cell culture, chicken embryos and laboratory animals and identification in RIF, ELISA.
For rapid identification of the virus in the material - RIF and PCR.
Serological method: Determination of virus-specific antibodies (IgA, IgM, IgG) in ELISA and RIA reactions. The serum of those who have been ill with herpes zoster contains more specific antibodies than the serum of those who have had chicken pox.
Treatment and prevention
Interferon, itch relievers, analgesics (menavazin). Acyclovir, vidarabine.
Live varicella vaccine.
Patients at high risk of severe infection are passively immunized varicella- zoster- Ig.
The patient is isolated at home, the isolation is terminated 5 days after the appearance of the last fresh element of the rash. Persons in the period "dried crusts" are not contagious and can be allowed in the team. Children of preschool age who are in contact with a sick person and have not had chicken pox are not allowed in childcare facilities from the 11th to the 21st day of contact.
Epstein-Barr virus:
HHV4.
1964 - Michelle Epstein And Evelyn Barr isolated the virus from Burkitt's lymphoma.
Burkitt's lymphoma- children 5-8 years old. The primary localization of the tumor is the upper jaw, which responds well to chemotherapy. Central Africa, Oceania.
Nasopharyngeal carcinoma(male population of China).
Intralab outbreak infectious mononucleosis.
EBV is found everywhere, most people become infected in childhood, by the age of three, 30-80% (in economically backward countries, almost 100% - the density of contacts) become carriers of EBV.
Epstein-Barr virus:
The virus has specific antigens:
EB-VCA - viral capsid AG,
EB-NA- nuclear AG,
EB-EA- early superficial hypertension,
EB-MA - membrane AG.
The detection of early surface and nuclear antigens indicates an acute infection with EBV, and the detection of late membrane and capsid antigens indicates a long-standing infection and latent infection.
cultural properties
The virus multiplies only in the culture of Burkitt's tumor lymphoblasts, in the blood cells of patients with infectious mononucleosis, leukemic cells, and in the culture of healthy human brain cells.
EBV can cause lymphoid neoplasia in marmosets (small Brazilian marmosets) and owl monkeys (the cat-like South American common night monkeys, or durukuli).
Pathogenesis of EBV infection:
Source of infection- a patient with asymptomatic or manifest forms, virus carriers (after the illness, the virus is shed from the nasopharyngeal swabs of many patients for up to 16 months).
Ways of infection:
airborne ("kissing disease");
fecal-oral mechanism, alimentary route (with the participation of food products contaminated with the virus);
contact household;
contact (sexual);
transfusion.
Stages of EBV infection:
latent viral persistence;
lytic viral replication.
Latent infection:
a constant number of copies of the genome;
limited gene expression;
episomal genome;
the possibility of neoplasms.
Lytic infection
acute stage of infection;
active reproduction of the virus;
cytopathology;
active release of the virus into the environment.
Cells affected by EBV
B and T lymphocytes;
epithelial cells of the nasopharynx;
glandular epithelium of the stomach, salivary glands, thyroid gland.
Infectious mononucleosis
generalized lymphadenopathy;
fever;
tonsillitis;
hepatosplenomegaly;
characteristic hematological changes (atypical mononuclear cells).
BURKITT'S LYMPHOMA- a malignant lymphoid tumor, localized, as a rule, outside the lymph nodes in various organs and tissues (upper jaw, kidneys, ovaries, liver, nervous system, etc.).
Microbiological diagnostics
In infectious mononucleosis, heterophilic antibodies to erythrocytes of various animals (sheep, horse, bull, etc.) appear in the course of the disease. In 1932 Paul and Bunnel proposed a reaction based on the detection of anti-sheep agglutinins in the blood serum of a patient.
cytological method researches of imprints from palatine tonsils. Atypical mononuclear cells - infectious mononucleosis.
Cytomegalovirus (CMV)
HHV5.
Giant or cytomegalic cells 25-40 microns in size with large intranuclear inclusions, limited from the nuclear membrane by a pale rim that does not perceive color (owl's eye).
Slow replication.
Low pathogenicity.
CMV infection is ubiquitous but rarely manifests clinically.
Pathogenesis:
Source infection - man.
Mechanisms infection: airborne, contact (including sexual), paraenteral, transplacental.
The virus has a pronounced tropism for tissues salivary glands(with a localized form, it is found only in the tissues of the salivary glands).
CMV affects cells of various organs and systems, persists for a long time in the body and is periodically released into the external environment.
infectious process: asymptomatic latent infection, or clinically manifest (localized or generalized forms).
Place of persistence monocytes and macrophages.
Postnatal infection almost always asymptomatically.
Infectious mononucleosis, hepatitis, pneumonia.
CMV is one of the main causative agents opportunistic infections: with a weakening of T-cell immunity (HIV, in patients taking immunosuppressants and cytostatics).
Pathology of the fetus and newborns with CMV infection
Intrauterine infection usually goes unnoticed. But in 5% of cases (more often with infection in the first two trimesters of pregnancy) develops cytomegalic disease- an acute form of infection with damage to internal organs.
Fetal developmental defects, hepatitis and hepatosplenomegaly, thrombocytopenic purpura (hemorrhagic syndrome), hydro- and microcephaly, choreoretinitis.
In about 15% of cases, a latent infection: newborns are mentally retarded and lose their hearing due to damage to the sensory centers of the auditory nerve.
The greatest risk of intrauterine CMV infection of the fetus and the development of severe forms of the disease is observed in cases where a pregnant woman suffers primary CMVI.
Microbiological diagnostics
Material: urine, blood, vaginal and cervical secretions.
cytological method: detection of specific cells in urine and saliva sediment. Large cells with a hyperchromic nucleus, intranuclear inclusions, the nucleus is surrounded by a light zone of enlightenment ("owl's eye").
Virological method: virus isolation on fibroblast culture, identification - RIF, PCR.
Serological method: pH, RNGA, ELISA, classes of immunoglobulins. AT to pathogens TOR C H infections.
Serological markers of CMVI
IgM to early early proteins
IgG to early early proteins
IgM to structural proteins
IgG to structural proteins
IgG avidity index
Treatment and prevention
Ganciclovir and foscanet, which inhibit the synthesis of viral DNA.
A foreign drug CYTOTECT (human immunoglobulin against CMV infection for intravenous administration, Germany) has been registered in Russia.
Herpes virus type 6
HHV-6.
According to various sources, from 80 to 94% of those examined have antibodies to this virus.
Probably involved in the development of roseola infantum (sudden exanthema) or pseudorubella in infants, neonatal erythema and chronic fatigue syndrome (CFS).
Microbiological diagnostics. Determination of viral DNA in PCR and accumulation of antiviral antibodies in ELISA.
Human herpes virus type 7
HHV-7.
The virus is distributed everywhere, but unevenly.
HHV-7 is a T-lymphotropic virus that has the ability to infect CD4 and CD8 lymphocytes and immature T cells.
An association has been suggested between the virus and CFS and VE in children.
Human herpes virus type 8
HHV-8.
In 1995, virus-like particles containing DNA with elements of homology with EBV were isolated from a biopsy specimen from a patient with Kaposi's sarcoma.
 n Herpes viruses (from the Greek. herpes - creeping) - DNA containing n Every year 20 million people are infected with HSV
n Herpes viruses (from the Greek. herpes - creeping) - DNA containing n Every year 20 million people are infected with HSV

 n alphaherpesvirinae a) human herpes simplex virus type I (HSV-1) HVV-1 b) human herpes simplex virus type II (HSV-2) HVV-2 c) varicella-zoster virus and herpes zoster HVV-3 genus Varicellovirus (VZV – Varicella-zoster virus)
n alphaherpesvirinae a) human herpes simplex virus type I (HSV-1) HVV-1 b) human herpes simplex virus type II (HSV-2) HVV-2 c) varicella-zoster virus and herpes zoster HVV-3 genus Varicellovirus (VZV – Varicella-zoster virus)
 n betaherpesvirinae a) cytomegalovirus (CMV) HHV-5 genus Cytomegalovirus b) infantile exanthema virus (affects children under 3 years old) HHV-6 c) chronic fatigue syndrome virus HHV-7
n betaherpesvirinae a) cytomegalovirus (CMV) HHV-5 genus Cytomegalovirus b) infantile exanthema virus (affects children under 3 years old) HHV-6 c) chronic fatigue syndrome virus HHV-7
 n gammaherpesvirinae a) Epstein-Barr virus (infectious mononucleosis and Burket's lymphoma) HHV-4 genus Lymphocryptovirus b) Kaposi's sarcoma-associated viruses HHV-8 genus Radinovirus
n gammaherpesvirinae a) Epstein-Barr virus (infectious mononucleosis and Burket's lymphoma) HHV-4 genus Lymphocryptovirus b) Kaposi's sarcoma-associated viruses HHV-8 genus Radinovirus
 Properties of viruses: n size 150 - 210 nm, spherical or oval shape n DNA linear, 2-stranded n icosahedral protein capsid, consists of 162 capsomeres n glycolipoprotein shell with glycoprotein spikes n tegument is located between the capsid and the glycoprotein shell - these are proteins, enzymes needed for replication
Properties of viruses: n size 150 - 210 nm, spherical or oval shape n DNA linear, 2-stranded n icosahedral protein capsid, consists of 162 capsomeres n glycolipoprotein shell with glycoprotein spikes n tegument is located between the capsid and the glycoprotein shell - these are proteins, enzymes needed for replication
 Virus reproduction n Virus envelope attaches to target cell membrane receptors n Fusion and entry by receptor endocytosis n Released nucleocapsid enters the cell nucleus. Transcription occurs (DNA in i. RNA), then i-RNA penetrates into the cytoplasm
Virus reproduction n Virus envelope attaches to target cell membrane receptors n Fusion and entry by receptor endocytosis n Released nucleocapsid enters the cell nucleus. Transcription occurs (DNA in i. RNA), then i-RNA penetrates into the cytoplasm
 The reproduction of the virus n begins the synthesis of non-structural (synthesis regulators and enzymes) and structural proteins (capsid, HP). GPs are adjacent to the nuclear membrane n the formed capsid is filled with DNA and buds through the nuclear membrane into the cytoplasm n exit occurs (exocytosis or cell lysis)
The reproduction of the virus n begins the synthesis of non-structural (synthesis regulators and enzymes) and structural proteins (capsid, HP). GPs are adjacent to the nuclear membrane n the formed capsid is filled with DNA and buds through the nuclear membrane into the cytoplasm n exit occurs (exocytosis or cell lysis)

 General properties for viruses of the subfamily alphaherpesvirinae Rapid growth n Proliferate in the epithelium of the skin and mucous membranes n Have a cytolytic effect n Remain in neurons n Cause latent persistent infection n
General properties for viruses of the subfamily alphaherpesvirinae Rapid growth n Proliferate in the epithelium of the skin and mucous membranes n Have a cytolytic effect n Remain in neurons n Cause latent persistent infection n
 General properties for viruses of the betaherpesvirinae subfamily Slow growth n Tropicity to the epithelium of the salivary glands, tonsils, kidneys, lymphocytes n Have cytomegalic (giant cells) and lymphoproliferative actions n
General properties for viruses of the betaherpesvirinae subfamily Slow growth n Tropicity to the epithelium of the salivary glands, tonsils, kidneys, lymphocytes n Have cytomegalic (giant cells) and lymphoproliferative actions n
 Common properties for viruses of the gammaherpesvirinae subfamily Grow only in lymphoblasts n Have a lymphoproliferative effect n Stimulate the reproduction of B-lymphocytes and cause persistent infection in them n Infect lymphoid tissue, salivary glands, epithelium of the mouth and pharynx n
Common properties for viruses of the gammaherpesvirinae subfamily Grow only in lymphoblasts n Have a lymphoproliferative effect n Stimulate the reproduction of B-lymphocytes and cause persistent infection in them n Infect lymphoid tissue, salivary glands, epithelium of the mouth and pharynx n
 Cultivation Depends on the specific virus chick embryo n cell lines (death, proliferation, nuclear inclusions - capsid residues detected by staining according to Romanovsky-Giemsa) n
Cultivation Depends on the specific virus chick embryo n cell lines (death, proliferation, nuclear inclusions - capsid residues detected by staining according to Romanovsky-Giemsa) n
 Antigenic structure Two antigenic complexes - n Capsid - group-specific n Glycoprotein - species-specific, type-specific
Antigenic structure Two antigenic complexes - n Capsid - group-specific n Glycoprotein - species-specific, type-specific
 General signs of herpesviruses n n n n Anthroponoses are not stable in the external environment. Polytropic - no strict organotropy Long-term persistence (chronic persistent infection with exacerbations) Immunosuppression (suppression of cellular immunity) Protection against the virus with the help of T-killers and macrophages that destroy the affected cells Antibodies do not have protective properties
General signs of herpesviruses n n n n Anthroponoses are not stable in the external environment. Polytropic - no strict organotropy Long-term persistence (chronic persistent infection with exacerbations) Immunosuppression (suppression of cellular immunity) Protection against the virus with the help of T-killers and macrophages that destroy the affected cells Antibodies do not have protective properties
 Subfamily alphaherpesvirinae Discovered by Grüter in 1912 1. HSV type I (acute stomatitis, keratoconjunctivitis, pharyngitis, meningoencephalitis) up to 10% of the population are carriers of this virus. Ways of transmission - airborne, contact (mother-child up to 3 years), transplacental. 2. HSV type II (herpes in newborns, genital herpes, cervical cancer). n Ways of transmission - sexual, during childbirth, infection of the child
Subfamily alphaherpesvirinae Discovered by Grüter in 1912 1. HSV type I (acute stomatitis, keratoconjunctivitis, pharyngitis, meningoencephalitis) up to 10% of the population are carriers of this virus. Ways of transmission - airborne, contact (mother-child up to 3 years), transplacental. 2. HSV type II (herpes in newborns, genital herpes, cervical cancer). n Ways of transmission - sexual, during childbirth, infection of the child
 Herpes Simplex Virus n Negative stain n Color photo Both viruses have CPD - blistering (vesicular eruptions) Immunity Ig M - fresh infection, Ig G - chronic or persistent.
Herpes Simplex Virus n Negative stain n Color photo Both viruses have CPD - blistering (vesicular eruptions) Immunity Ig M - fresh infection, Ig G - chronic or persistent.
 Subfamily alphaherpesvirinae HSV 1 and HSV 2 Laboratory diagnostics n Test material: scraping from vesicles, saliva, swab from the cervical canal in case of genital herpes, blood in case of generalization, cerebrospinal fluid in case of meningitis or encephalitis. n Express diagnostics. RIF, PCR, microscopy (intracellular inclusions and giant multinucleated cells)
Subfamily alphaherpesvirinae HSV 1 and HSV 2 Laboratory diagnostics n Test material: scraping from vesicles, saliva, swab from the cervical canal in case of genital herpes, blood in case of generalization, cerebrospinal fluid in case of meningitis or encephalitis. n Express diagnostics. RIF, PCR, microscopy (intracellular inclusions and giant multinucleated cells)
 Subfamily alphaherpesvirinae HSV 1 and HSV 2 Laboratory diagnostics n Virological method - chicken embryo - CAO (plaques), infection of mice into the brain (encephalitis), rabbits into the cornea of the eye (keratitis), culture of rabbit kidney cells (giant cells with intranuclear inclusions) Identification by RN, RSK, ELISA n Serodiagnosis by ELISA (IG M, G)
Subfamily alphaherpesvirinae HSV 1 and HSV 2 Laboratory diagnostics n Virological method - chicken embryo - CAO (plaques), infection of mice into the brain (encephalitis), rabbits into the cornea of the eye (keratitis), culture of rabbit kidney cells (giant cells with intranuclear inclusions) Identification by RN, RSK, ELISA n Serodiagnosis by ELISA (IG M, G)
 Subfamily alphaherpesvirinae HSV 1 and HSV 2 Specific relapse prevention: Herpes therapeutic culture-inactivated vaccine (reduces relapse rate but does not cure). n Treatment: virolex, acyclovir, famvir. n
Subfamily alphaherpesvirinae HSV 1 and HSV 2 Specific relapse prevention: Herpes therapeutic culture-inactivated vaccine (reduces relapse rate but does not cure). n Treatment: virolex, acyclovir, famvir. n
 Subfamily alphaherpesvirinae 3. n n Varicella-zoster virus (VZV) or GVV-3 (chickenpox and shingles) discovered by Arago (Brazilian doctor) in 1911 Chickenpox has an epidemic distribution
Subfamily alphaherpesvirinae 3. n n Varicella-zoster virus (VZV) or GVV-3 (chickenpox and shingles) discovered by Arago (Brazilian doctor) in 1911 Chickenpox has an epidemic distribution
 Subfamily alphaherpesvirinae Virus Varicella-zoster Pathogenesis Primary reproduction in the mucous membrane of the upper respiratory tract (incubation period - 10-15 days). Viremia Secondary reproduction - in the epithelium of the mucous membranes and skin (cytopathic effect)
Subfamily alphaherpesvirinae Virus Varicella-zoster Pathogenesis Primary reproduction in the mucous membrane of the upper respiratory tract (incubation period - 10-15 days). Viremia Secondary reproduction - in the epithelium of the mucous membranes and skin (cytopathic effect)
 Subfamily alphaherpesvirinae Virus Varicella-zoster n Formation of a bladder with serous fluid (vesicle) n Suppuration (pustule) is possible n Scar formation (pockmark) There is constant underseeding from reproduction sites, there can be up to 5 or more attacks, and the patient can see all the elements of the rash. In debilitated patients - bullous form (huge blisters), hemorrhagic form and gangrenous form.
Subfamily alphaherpesvirinae Virus Varicella-zoster n Formation of a bladder with serous fluid (vesicle) n Suppuration (pustule) is possible n Scar formation (pockmark) There is constant underseeding from reproduction sites, there can be up to 5 or more attacks, and the patient can see all the elements of the rash. In debilitated patients - bullous form (huge blisters), hemorrhagic form and gangrenous form.
 Subfamily alphaherpesvirinae Virus Varicella-zoster Epidemiology n 100% contagiousness n Way of transmission - airborne, can be contact (rarely, because it is not very resistant) n Susceptible group - adults and children in the absence of immunity
Subfamily alphaherpesvirinae Virus Varicella-zoster Epidemiology n 100% contagiousness n Way of transmission - airborne, can be contact (rarely, because it is not very resistant) n Susceptible group - adults and children in the absence of immunity
 Subfamily alphaherpesvirinae Virus Varicella-zoster Laboratory diagnostics Test material - nasopharyngeal lavage and discharge of vesicles n Express diagnostics - ELISA n Virological - culture of human embryonic fibroblasts (HRC). n Serodiagnosis - RSK, RTGA, ELISA.
Subfamily alphaherpesvirinae Virus Varicella-zoster Laboratory diagnostics Test material - nasopharyngeal lavage and discharge of vesicles n Express diagnostics - ELISA n Virological - culture of human embryonic fibroblasts (HRC). n Serodiagnosis - RSK, RTGA, ELISA.
 Alphaherpesvirinae subfamily Varicella-zoster virus Specific prophylaxis Live attenuated vaccines Okavax (Japan), Varilrix (England) Human immunoglobulin against convalescents n Treatment - interferon, leukinferon, virolex n
Alphaherpesvirinae subfamily Varicella-zoster virus Specific prophylaxis Live attenuated vaccines Okavax (Japan), Varilrix (England) Human immunoglobulin against convalescents n Treatment - interferon, leukinferon, virolex n
 Subfamily betaherpesvirinae 1. Cytomegalovirus infection (HVV 5) n According to WHO, 1-2% of children are born with this infection, by the age of 1 year, 20% of children have antibodies, by 30-50 years - 100% of antibodies n Identified in 1956 in the USA by Smith and Rod n Morphology - large sizes of DNA, changes the rate of cell growth, with the formation of giant multinucleated cells with inclusions in the nucleus
Subfamily betaherpesvirinae 1. Cytomegalovirus infection (HVV 5) n According to WHO, 1-2% of children are born with this infection, by the age of 1 year, 20% of children have antibodies, by 30-50 years - 100% of antibodies n Identified in 1956 in the USA by Smith and Rod n Morphology - large sizes of DNA, changes the rate of cell growth, with the formation of giant multinucleated cells with inclusions in the nucleus
 Subfamily betaherpesvirinae n Pathogenesis Reproduction in leukocytes and macrophages with long persistence n Epitheliotropism (salivary glands and kidneys) n Formation of infiltrates that are replaced by fibrous tissue
Subfamily betaherpesvirinae n Pathogenesis Reproduction in leukocytes and macrophages with long persistence n Epitheliotropism (salivary glands and kidneys) n Formation of infiltrates that are replaced by fibrous tissue
 Subfamily betaherpesvirinae n n Clinical features Congenital CMV - when infected in early pregnancy, the fetus dies or birth defects. In the later stages - loss of vision, hearing, etc. Acquired CMV - acute (in young children, at the time of birth) or chronic infection (hepatolienal syndrome, kidney damage) In the later stages - asymptomatic infection with the formation of antibodies
Subfamily betaherpesvirinae n n Clinical features Congenital CMV - when infected in early pregnancy, the fetus dies or birth defects. In the later stages - loss of vision, hearing, etc. Acquired CMV - acute (in young children, at the time of birth) or chronic infection (hepatolienal syndrome, kidney damage) In the later stages - asymptomatic infection with the formation of antibodies
 Subfamily betaherpesvirinae Epidemiology n Source of infection - patients or virus carriers (viruses are found in all biological fluids) n Ways of transmission - transplacental, through amniotic fluid, contact, airborne, sexual
Subfamily betaherpesvirinae Epidemiology n Source of infection - patients or virus carriers (viruses are found in all biological fluids) n Ways of transmission - transplacental, through amniotic fluid, contact, airborne, sexual
 Subfamily betaherpesvirinae Laboratory diagnostics - in urine and saliva of cytomegalocellular cells n Virological method - culture of human embryonic fibroblasts (HRC, RN). n Serological method - ELISA, separately antibodies M and G, M - fresh infection.
Subfamily betaherpesvirinae Laboratory diagnostics - in urine and saliva of cytomegalocellular cells n Virological method - culture of human embryonic fibroblasts (HRC, RN). n Serological method - ELISA, separately antibodies M and G, M - fresh infection.
 Subfamily betaherpesvirinae n n Specific prophylaxis No vaccine yet Treatment - specific immunoglobulin - cytotect, used to treat pregnant women and newborns
Subfamily betaherpesvirinae n n Specific prophylaxis No vaccine yet Treatment - specific immunoglobulin - cytotect, used to treat pregnant women and newborns
 Subfamily betaherpesvirinae 2. Infant exanthema virus HHV-6 n Discovered in 1986. Halo n T-lymphotropic virus - exanthema in infants with a sudden rise in temperature to 40 ° C. With and the same recession on the background of a rash.
Subfamily betaherpesvirinae 2. Infant exanthema virus HHV-6 n Discovered in 1986. Halo n T-lymphotropic virus - exanthema in infants with a sudden rise in temperature to 40 ° C. With and the same recession on the background of a rash.
 Subfamily betaherpesvirinae 3. Chronic fatigue syndrome virus HHV-7 n Discovered by Frenkel in 1990 n T-lymphotropic virus - causes chronic fatigue syndrome (subfebrile arthralgia, weakness)
Subfamily betaherpesvirinae 3. Chronic fatigue syndrome virus HHV-7 n Discovered by Frenkel in 1990 n T-lymphotropic virus - causes chronic fatigue syndrome (subfebrile arthralgia, weakness)
 Subfamily gammaherpesvirinae 1. Epstein-Barr virus (EBV or HHV-4) was discovered in 1964 and causes infectious mononucleosis. n Described by Filatov more than 100 years ago. n Can cause malignant diseases - Burkitt's lymphoma (a tumor of the upper jaw in young Africans) when tropical conditions and Plasmodium malaria or nasopharyngeal carcinoma with recurrent mumps play a role. n May have B-cell leukemia.
Subfamily gammaherpesvirinae 1. Epstein-Barr virus (EBV or HHV-4) was discovered in 1964 and causes infectious mononucleosis. n Described by Filatov more than 100 years ago. n Can cause malignant diseases - Burkitt's lymphoma (a tumor of the upper jaw in young Africans) when tropical conditions and Plasmodium malaria or nasopharyngeal carcinoma with recurrent mumps play a role. n May have B-cell leukemia.
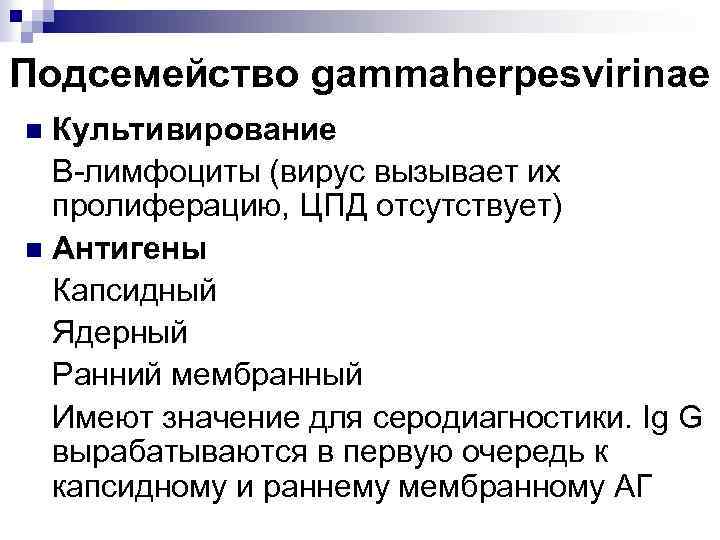 Subfamily gammaherpesvirinae Cultivation B-lymphocytes (the virus causes them to proliferate, there is no CPP) n Antigens Capsid Nuclear Early membranous Significant for serodiagnosis. Ig G are produced primarily to capsid and early membrane hypertension n
Subfamily gammaherpesvirinae Cultivation B-lymphocytes (the virus causes them to proliferate, there is no CPP) n Antigens Capsid Nuclear Early membranous Significant for serodiagnosis. Ig G are produced primarily to capsid and early membrane hypertension n
 Subfamily gammaherpesvirinae n Pathogenesis. Infection of the immune system. primary reproduction (mucosa of the oral cavity and nasopharynx) secondary reproduction occurs in B-lymphocytes, which leads to hyperplasia of the lymphoid tissue of the nasopharynx, polylymphadenopathy, hepatosplenomegaly May be self-healing Immunodeficiency may lead to the development of Burkitt's lymphoma (a malignant tumor consisting of B-lymphocytes, mainly in the brain )
Subfamily gammaherpesvirinae n Pathogenesis. Infection of the immune system. primary reproduction (mucosa of the oral cavity and nasopharynx) secondary reproduction occurs in B-lymphocytes, which leads to hyperplasia of the lymphoid tissue of the nasopharynx, polylymphadenopathy, hepatosplenomegaly May be self-healing Immunodeficiency may lead to the development of Burkitt's lymphoma (a malignant tumor consisting of B-lymphocytes, mainly in the brain )
 Subfamily gammaherpesvirinae n Epidemiology. The disease is not contagious. Source - patients and virus carriers Ways of infection transmission - airborne, contact-household (with a kiss), transplacental (during childbirth) EBV was found in saliva, cervical secretion Mostly men from 14 to 29 years old get sick
Subfamily gammaherpesvirinae n Epidemiology. The disease is not contagious. Source - patients and virus carriers Ways of infection transmission - airborne, contact-household (with a kiss), transplacental (during childbirth) EBV was found in saliva, cervical secretion Mostly men from 14 to 29 years old get sick
 Subfamily gammaherpesvirinae Laboratory diagnostics. n Express diagnostics. PCR for the detection of DNA in various biological fluids. ELISA. n Serodiagnostics. ELISA for the detection of antibodies (Ig. M to capsid AG - fresh infection) Specific prophylaxis. Absent
Subfamily gammaherpesvirinae Laboratory diagnostics. n Express diagnostics. PCR for the detection of DNA in various biological fluids. ELISA. n Serodiagnostics. ELISA for the detection of antibodies (Ig. M to capsid AG - fresh infection) Specific prophylaxis. Absent
 Herpes simplex virus Type 1 (HSV-1) Herpes simplex virus Type 2 (HSV-2) Epstein Barr virus (EBV) Cytomegalovirus (CMV) Varicella Zoster Virus (VZV) Human herpes virus 6 (exanthum subitum) or roseola infantum) Human herpes virus 8 (Kaposi's sarcoma-associate herpes virus)
Herpes simplex virus Type 1 (HSV-1) Herpes simplex virus Type 2 (HSV-2) Epstein Barr virus (EBV) Cytomegalovirus (CMV) Varicella Zoster Virus (VZV) Human herpes virus 6 (exanthum subitum) or roseola infantum) Human herpes virus 8 (Kaposi's sarcoma-associate herpes virus)

 n n n TABLE 2 - Properties of Herpes viruses Human herpes type Name Sub Family Target cell type Latency Transmission 1 Herpes simplex-1 (HSV-1) Alphaherpesvirinae Mucoepithelia Neuron Close contact 2 Herpes simplex-2 (HSV-2) Alphaherpesvirinae Mucoepithelia Neuron Close contact usually sexual 3 Varicella Zoster virus (VSV) Alphaherpesvirinae Mucoepithelia Neuron Contact or respiratory route 4 Epstein-Barr Virus (EBV) Gammaherpesvirinae B lymphocyte, epithelia B lymphocytes Saliva 5 Cytomegalovirus (CMV) Betaherpesvirinae Epithelia, monocytes, lymphocytes Monocytes, lymphocytes and possibly others Contact, blood transfusions, transplantation, congenital 6 Herpes lymphotropic virus Betaherpesvirinae T lymphocytes and others Contact, respiratory route 7 Human herpes virus-7 (HHV-7) Betaherpesvirinae T lymphocytes and others Unknown 8 Human herpes virus-8 (HHV-8) Kaposi's sarcoma-associated herpes virus (KSHV) Gammaherpesvirinae Endothelial cells Exchange of body fluids?
n n n TABLE 2 - Properties of Herpes viruses Human herpes type Name Sub Family Target cell type Latency Transmission 1 Herpes simplex-1 (HSV-1) Alphaherpesvirinae Mucoepithelia Neuron Close contact 2 Herpes simplex-2 (HSV-2) Alphaherpesvirinae Mucoepithelia Neuron Close contact usually sexual 3 Varicella Zoster virus (VSV) Alphaherpesvirinae Mucoepithelia Neuron Contact or respiratory route 4 Epstein-Barr Virus (EBV) Gammaherpesvirinae B lymphocyte, epithelia B lymphocytes Saliva 5 Cytomegalovirus (CMV) Betaherpesvirinae Epithelia, monocytes, lymphocytes Monocytes, lymphocytes and possibly others Contact, blood transfusions, transplantation, congenital 6 Herpes lymphotropic virus Betaherpesvirinae T lymphocytes and others Contact, respiratory route 7 Human herpes virus-7 (HHV-7) Betaherpesvirinae T lymphocytes and others Unknown 8 Human herpes virus-8 (HHV-8) Kaposi's sarcoma-associated herpes virus (KSHV) Gammaherpesvirinae Endothelial cells Exchange of body fluids?










The main differences in the reproductive cycle herpesviruses from other DNA viruses associated with a more complex structure of the genome. Adsorption of viruses on cells is carried out through specific receptors. After interacting with receptors, the viral envelope fuses with cell membrane and the nucleocapsid is released into the cytoplasm. The undressing (deproteinization) of the viral genome occurs at the nuclear membrane, and the viral DNA ends up in the nucleus of the host cell. Reproduction includes early and late stages, but they are not clearly distinguished.
Early stage of reproduction of herpesviruses. In the early stage, "early proteins" are synthesized, encoded by the proximal third of the DNA molecule. They exhibit regulatory properties, including activation of transcription of other regions of the viral genome encoding DNA polymerase and DNA-binding proteins.
Late stage of reproduction of herpesviruses. In the late stage, viral DNA polymerase induces replication of maternal DNA. As a result, DNA molecules of the daughter population are formed. Part of the daughter DNA is read by cellular polymerases, which causes the transcription of terminal genes encoding structural proteins (envelope proteins and spike glycoproteins).
Assembly of daughter populations of herpesviruses is carried out in the nucleus, where capsid proteins surround DNA molecules, forming nucleocapsids. The final stage of herpesvirus morphogenesis is the formation of a supercapsid on the inner surface of the nuclear membrane. Mature daughter populations bud from the modified nuclear membrane, are transported through the cytoplasm, and are released to the outside.
poxviruses have the most complex reproductive cycle, while more than 100 different proteins that make up the virions are synthesized (the majority forms the outer shell). The reproduction of poxviruses is characterized by the following features.
DNA transcription begins before the complete deproteinization of the virus, since it is completely carried out by viral polymerases.
replication occurs only in the cytoplasm and is completely independent of cellular polymerases, since, unlike other viruses, poxviruses have their own DNA-dependent RNA polymerase, which ensures that more than half of the viral genome is read during the initial and early stages.
In the reproductive cycle There are three stages - initial, early and late.
 Rice. 5-4. Replication cycle of DNA-containing viruses(on the example of the reproduction of the herpes virus). After adsorption (1), the virus enters the cell by fusion with the membrane (2). The nucleocapsid is transported to the nuclear envelope (3), and the viral DNA (vDNA) enters the cell nucleus, where its transcription by the cellular DNA-dependent RNA polymerase begins (4). The "early genes" are transcribed first. As a result of translation of the "early portion" of the viral genome, "early proteins" are synthesized (5), including regulatory, template, and viral polymerases. Viral polymerase penetrates into the cell genome (6), where it triggers the synthesis of DNA molecules of daughter populations (7). Part of the viral DNA (“late genes”) of daughter populations is transcribed by cellular RNA polymerase (8), which leads to the synthesis of “late proteins” (9) necessary for the assembly of daughter populations (10). The latter leave the nucleus, budding from its membrane (11), fragments of which they contain in their shell.
Rice. 5-4. Replication cycle of DNA-containing viruses(on the example of the reproduction of the herpes virus). After adsorption (1), the virus enters the cell by fusion with the membrane (2). The nucleocapsid is transported to the nuclear envelope (3), and the viral DNA (vDNA) enters the cell nucleus, where its transcription by the cellular DNA-dependent RNA polymerase begins (4). The "early genes" are transcribed first. As a result of translation of the "early portion" of the viral genome, "early proteins" are synthesized (5), including regulatory, template, and viral polymerases. Viral polymerase penetrates into the cell genome (6), where it triggers the synthesis of DNA molecules of daughter populations (7). Part of the viral DNA (“late genes”) of daughter populations is transcribed by cellular RNA polymerase (8), which leads to the synthesis of “late proteins” (9) necessary for the assembly of daughter populations (10). The latter leave the nucleus, budding from its membrane (11), fragments of which they contain in their shell.
The initial stage of reproduction of poxviruses starts immediately after the undressing of the virus and the release of viral DNA into the cytoplasm.
Early stage of poxvirus reproduction. At this stage, approximately half of the viral DNA is transcribed. Enzymes encoded by "early genes" and involved in viral DNA replication are synthesized. In parallel, structural proteins are formed in a small amount.
Late stage of poxvirus reproduction coincides with the start of DNA replication (which switches transcription mechanisms to read the second half of the genome). Regulatory proteins block the translation of "early mRNA" and trigger the synthesis of late (structural) proteins. Virions are assembled only in the cytoplasm through membrane synthesis reactions. The release of mature populations is accompanied by cell lysis.
Herpesviruses (from the Greek herpes - creeping) are a family of large enveloped DNA-containing viruses that cause a variety of infections.
The Herpesviridae family includes three subfamilies that differ in genome structure, tissue tropism, cytopathology, and localization of latent infection:
Structure. The herpesvirus virion has an oval shape with a diameter of 150-200 nm.
In the central part of the virion there is a double-stranded linear DNA surrounded by an icosahedral capsid consisting of 162 capsomeres. Outside, the virus is surrounded by a shell with glycoprotein spikes formed from the inner layer of the cell's nuclear membrane. The space between the capsid and the shell is called tegument(contains viral proteins and enzymes necessary to initiate replication). The genome is double-stranded linear DNA. It consists: in HSV and CMV, of two fragments: short S and long L, each of which in HSV is enclosed between two sets of inverted repeats, allowing the genome to recombine to form 4 isomers; in VZV DNA also consists of two fragments: short S and long L, but contains one set of inverted repeats, so two isomeric forms are formed.
Reproduction.

After attaching to cell receptors, the virion envelope fuses with the cell membrane (1, 2). The released nucleocapsid (3) delivers the virus DNA to the cell nucleus. Next, transcription of a part of the viral genome occurs (using cellular DNA-dependent RNA polymerase); the formed mRNA (4) penetrate into the cytoplasm where the synthesis (translation) of the earliest alpha proteins (I) with regulatory activity takes place. Then, early beta proteins (P) are synthesized - enzymes, including DNA-dependent DNA polymerase and thymidine kinase, involved in the replication of the genomic DNA of the virus. Late gamma proteins (III) are structural proteins including the capsid and glycoproteins (A, B, C, D, E, F, G, X). Glycoproteins diffusely adhere to the nuclear envelope (5). The emerging capsid (6) is filled with viral DNA and buds through the modified membranes of the nuclear envelope (8). Moving through the Golgi apparatus, virions are transported through the cytoplasm and exit the cell by exocytosis (9) or cell lysis (10).
herpes simplex virus belongs to the Herpesviridae family, genus Simplexvirus. It causes herpes simplex, characterized by vesicular rashes on the skin, mucous membranes, damage to the central nervous system and internal organs, as well as lifelong carriage (persistence) and relapses of the disease. The herpes simplex virus includes two types: HSV-1 and HSV-2; It is ubiquitous, affects most of the world's population and exists in the body in a latent form until reactivation.
HSV-1 mainly affects the mouth, eyes, central nervous system, and HSV-2 affects the genitals, for which it received the name genital strain.